 There is no doubt that today more and more people are turning to integrative medicine and alternative modalities for their health concerns and disease prevention. This popular movement, winning one out of every two Americans as converts, may seem to some like a new idea or a “health revolution”. In reality, it is in a return to period in time, over 400 years ago, when health was seen from a more whole person, integrated and even spiritual perspective.
There is no doubt that today more and more people are turning to integrative medicine and alternative modalities for their health concerns and disease prevention. This popular movement, winning one out of every two Americans as converts, may seem to some like a new idea or a “health revolution”. In reality, it is in a return to period in time, over 400 years ago, when health was seen from a more whole person, integrated and even spiritual perspective.
Until the early 1600’s, the realm of human health was believed to represent a person’s spiritual state. If one was healthy that meant they bore not demons. If one was sick, that meant they needed to purge sickness, which was seen as “possession” or a spiritual incorrectness that had to be remedied. The prevailing church of the day, ruled by the Vatican, exerted a huge influence over the medical community and how people viewed the cause and cure of their disease.
In 1612, physician Anton Descartes, a powerful, influential physician and scientist, declared, “I think therefore I am” , stating that the mind and body were two separate, unrelated parts of a human being, and as such the study and treatment of the human being needed to be separated into the mind or spirit portion and the physical bodily portion.
Descartes lead the political movement to separate the body from the soul, a separation in which he and his peers literally brokered a deal with the Vatican, which was reluctant to give up control over its flock. However, the “scientific revolution” was gripping the culture and the church knew it was prudent to agree. Thus, the division of mind and body began and the practice of medicine started down the slippery slope to where we find ourselves today.
Since this division set up a medical system that treated only physical health, it became considered, by the mass majority, that this form of medicine was the only legitimate form of health care. However, over the course of the past 50 years people have grown sicker and increasingly dissatisfied with the medical system.
This led to an increase in the use of “untried” remedies and treatments which offered success and often cures for varied ailments. These “alternatives” treatments attempt to address the whole person rather than just the physical body. Because of the success of alternative treatments, and their resultant popularity, we are currently experiencing a renaissance of the “whole-person” body, mind and spirit approach to healing.
Today, thanks to the Internet, we have more information about every aspect of health than ever before. Still, there exists confusion between alleopathic medicine and integrative medicine, how their treatment approaches differ and how one can discern what is right for their particular need or condition. By comparing and contrasting both approaches individuals can be empowered with information to make an educated decision about how they would like to address their personal health care and what forms of health care they would like to incorporate.
Often called modern medicine, conventional or traditional, allopathic medicine defines health as the absence of disease. The term comes from the Greek roots meaning “opposite” and “disease”, referring to a principle of curing a disease, disorder or problem by administering drugs or surgery that produce the opposite effect of the problem.
The main cause of illness is considered to be viruses or bacteria and scientific tests are used to diagnose before drugs or surgery are prescribed. Furthermore, the emphasis here is more on “attacking the problem”, seen as an invader or enemy outside the self rather than exploring the cause and effect of the problem and working to identifying what needs to be changed or altered to bring about the return of health.
Alternative, natural, complementary or holistic medicine practices approach the problem or condition from a focus of identifying what particular choices or behaviors the individual might be making that is leading to the expression of symptoms collectively called their “disease or diagnosis”.
In contrast, because integrative medicine bridges the gap between traditional and alternative medicine, an integrative physician or practitioner would evaluate not only the patient’s physical health, but also the other aspects of their life that may be influencing their health.
Scientific evidence and ancient teachings have proven that there are multiple components to health that make up a whole person, therefore, illness cannot be cured or wellness realized without taking multiple aspects into account.
For example, a traditional alleopathic approach to a sore throat could include a drug substance or over the counter aspirin and possibly a cough and sore throat medicine. The integrative medical practitioner, trained to stimulate the body’s natural healing potential, may well prescribe nutritional changes, herbs, aromatherapy, gargling with various natural extracts, vitamins, garlic, broths, vegetable or juice extracts, calcium sources or homeopathic remedies.
By looking at different patient situations we can see how traditional and integrative medicine differs in their approach. Patient A is a 35-year old male who is married with two children and works in a high stress job. He considers himself healthy however, despite working out fairly regularly and eating healthy, he is constantly tired and has trouble sleeping at night.
On the opposite end of the spectrum Patient B is a 50-year old single stay-at-home mom who is raising a young son. She has high cholesterol, is borderline diabetic and is generally not in good health.
Patient A: Conventional Analysis & Treatment Recommendation: This patient would most likely be given a blood test to check for anemia or pathology and then prescribed a sleeping pill to deal with the insomnia. If nothing showed up on the blood test, the practitioner would probably recommend addressing the stress with a pill to calm down to seeing a therapist to deal with his stress.
Patient A: Integrative Analysis & Treatment Recommendation: This practitioner would also probably order a blood test to check for anemia or pathology. After assessing that possibility, if the blood test came back “negative” (ironically, that’s positive!), the practitioner would then explore and discuss with the individual what they felt is contributing to their problem. Based on the patients’ self-awareness and the practitioners mindful listening and assessment of the patient, the practitioner might recommend a homeopathic remedy, a change in sleep venue or a new bed, meditation before retiring, an decrease in stimulating food such as caffeine and alcohol, and an increase in fruits and vegetables in t he diet. The multiple aspects of the individual’s life and their own innate awareness of their health would be considered.
Patient B: Conventional Analysis & Treatment Recommendation:This patient would be given a blood work-up to determine her levels of cholesterol and glucose or blood sugar. Depending upon the values found on the tests, the doctor would prescribe medications appropriate for lowering the levels of cholesterol and/or blood sugar. The doctor may also suggest the patient make an appointment with a dietician to go over dietary changes.
Patient B: Integrative Analysis & Treatment Recommendation: This practitioner would also do a blood work-up to assess the patient’s various blood values. However, rather than prescribing a drug to lower or later levels, this practitioner may invite the individual into a discussion about what she felt she could do to bring these levels down to avoid the need for a medication.
The discussion would outline and recommend options for lowering cholesterol which would include natural supplements, dietary changes or adding more vegetables and whole sprouted grains instead of high fat foods, an exercise program that she would be able to follow, drinking more water, using homeopathic remedies to improve her overall health, discuss her social life and recreation. This practitioner would focus on changing the causes of her chronic condition rather than just medicate it.
The options we are offered today through Integrative Medicine invite us to become more pro-active and better informed as well as become better health care consumers. This empowers us to take greater control over our health outcomes and longevity. That’s a prescription for good health we can all live with.
For more information on integrative whole health and nutrition, Watch Two Hours of FREE Whole Health Course Excerpts from the National Institute of Whole Health.


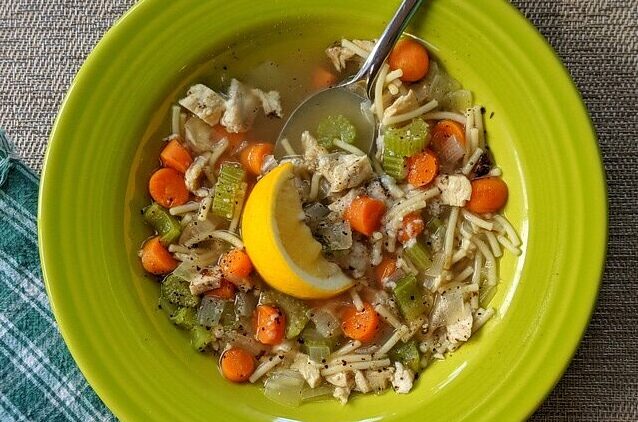 This cold and flu season it is likely with the recall of so many over the counter cold remedies, that home-made cold remedies will make a comeback this winter. One of the best known and oldest home-made remedies for “the winter miseries” is chicken soup.
This cold and flu season it is likely with the recall of so many over the counter cold remedies, that home-made cold remedies will make a comeback this winter. One of the best known and oldest home-made remedies for “the winter miseries” is chicken soup.

 There is no doubt that today more and more people are turning to integrative medicine and alternative modalities for their health concerns and disease prevention. This popular movement, winning one out of every two Americans as converts, may seem to some like a new idea or a “health revolution”. In reality, it is in a return to period in time, over 400 years ago, when health was seen from a more whole person, integrated and even spiritual perspective.
There is no doubt that today more and more people are turning to integrative medicine and alternative modalities for their health concerns and disease prevention. This popular movement, winning one out of every two Americans as converts, may seem to some like a new idea or a “health revolution”. In reality, it is in a return to period in time, over 400 years ago, when health was seen from a more whole person, integrated and even spiritual perspective.